Complications of cirrhosis
In the early stages of cirrhosis, symptoms are often subtle. Sometimes, in some people, complications are the first sign of the disease. The important thing is to recognize them early so that complications can be treated promptly and, best of all, how to prevent them from occurring.
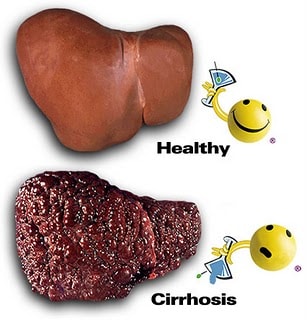 |
Cirrhosis is a chronic liver disease with a high mortality rate after liver cancer. This is the final consequence of chronic liver diseases, in which liver cells are damaged and replaced by fibrous tissue bands and “regenerated” nuclei that disrupt the normal structure of the liver, affecting the liver’s function. Basically, liver fibrosis cannot be reversed, however, if detected and treated early, it can stop the progression of the disease and limit complications.
Causes
There are many causes of cirrhosis such as: hepatitis B virus, hepatitis C virus, alcohol and toxins... In some countries, obesity is becoming one of the causes that can lead to cirrhosis. In our country, some common causes of cirrhosis: hepatitis B virus, hepatitis C virus and alcohol.
When liver function is severely impaired, it will lead to decompensated cirrhosis, at which point complications will appear frequently and the mortality rate can be up to 85% within 5 years if there is no liver transplant or if not treated actively and properly.
Some common complications in cirrhosis
Gastrointestinal bleeding due to ruptured esophageal varices:
Cirrhosis of the liver causes blood flow through the liver to be obstructed, leading to increased pressure in the portal vein as well as in the porta-systemic junction, especially causing dilation of the esophageal veins and gastric varices. When these veins are too dilated, they will rupture, causing vomiting of large amounts of bright red blood and passing bloody stools. If not treated promptly, it can easily lead to death. The patient needs to be taken to the emergency room immediately.
Treatment includes: blood transfusion, drug infusion to reduce portal vein pressure such as using somatostatin, octreotide, terlipressin, emergency gastroscopy to ligate or inject sclerosing varices. When the bleeding is stable, non-selective beta-blockers (propranolol) should be continued or nitrates can be added to prevent recurrent bleeding.
Leg edema and abdominal distention:
Portal hypertension and hypoproteinemia can lead to leg swelling and fluid accumulation in the abdomen (ascites). Moderate and severe ascites are at risk of infection, at which time the patient may have fever, abdominal pain, and loose stools. Ascites is also a symptom of decompensated liver failure. The patient needs to be hospitalized, treated with diuretics, and albumin infusion.
Hepatic coma or hepatic encephalopathy:
Cirrhotic liver cannot eliminate toxins in the body. Therefore, in severe cirrhosis, harmful toxins in the intestines - especially NH3 (ammonia) - enter the blood and accumulate in the brain, causing hepatic encephalopathy with symptoms of perceptual disorders ranging from confusion to hepatic coma and death. Hepatic encephalopathy can be triggered by a number of factors such as gastrointestinal bleeding, infection, constipation, dehydration, abuse of sleeping pills or sedatives, etc.
Treatment is mainly to reduce the amount of NH3 accumulated in the blood by limiting protein supply during coma, taking lactulose laxative to prevent NH3 absorption from the digestive tract, and using drugs to enhance liver detoxification to prevent toxins from affecting the nervous system.
 |
Liver cancer:
Cirrhosis caused by viral hepatitis B and C, alcohol, hemochromatosis and primary biliary cirrhosis can easily progress to liver cancer. Patients may not have any specific symptoms until a tumor is accidentally discovered in the liver during a health check-up and abdominal ultrasound. In the late stage: the tumor is too large, causing pain in the right subcostal region, weight loss, exhaustion or abdominal bleeding due to a ruptured tumor. For patients with cirrhosis, the most important thing is to monitor and screen for liver cancer every 3-6 months by doing an abdominal ultrasound and a blood test to quantify AFP to detect liver cancer early.
Infection status:
The liver participates in immune functions that protect the body against infection. Therefore, patients with cirrhosis are susceptible to infections, such as ascites, pneumonia, blood infections, etc. Infections can worsen liver disease and promote other complications such as hepatic coma, kidney failure, etc.
How to prevent complications of cirrhosis?
Preventive measures for some common complications of cirrhosis include:
- Edema and ascites: low-salt diet combined with diuretics.
- Gastrointestinal bleeding due to ruptured esophageal varices: use drugs to reduce portal vein pressure, ligate varices, or inject sclerotherapy, place portal-systemic stents in the liver.
- Infections: antibiotics, vaccinations against flu, pneumonia and hepatitis.
- Liver cancer: abdominal ultrasound and AFP test every 3-6 months.
- Hepatic encephalopathy: use lactulose laxative to avoid constipation and reduce NH3 toxicity in the blood.
According to health and life