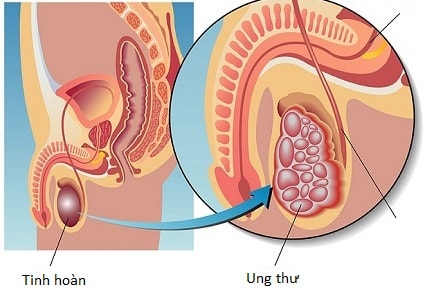
Signs of testicular cancer
For more than 30 years, the number of cases of testicular cancer has increased significantly. However, people should not panic because this disease is enjoying great achievements of biochemical treatment, changing the nature of the disease prognosis, with a cure rate of more than 95%.
Although not the most common type of urological cancer, testicular cancer, which usually occurs after puberty, has become the most common cancer in young people aged 20-35. The average incidence is 6 cases/100,000 people.
Some of the predisposing factors for testicular cancer are undescended testicles, germ cell dysplasia including testicular atrophy and infertility disorders. Some environmental factors, especially hormonal, originating from endocrine imbalance during the fetal period can also become favorable conditions for the disease.
How to detect the disease?
The disease can be easily diagnosed by self-examination of the scrotum, which reveals a testicular mass. Previously, joint examinations between schools and hospitals allowed the detection of testicular cancer in young men. In cases where the diagnosis is difficult, ultrasound combined with color Doppler ultrasound helps confirm the diagnosis.
Some blood tests are specific for germinal tumors such as Alpha-phoeto-proteine and human chorionic gonadotrophin (HCG). These tests confirm the diagnosis and, if high, allow prognosis and are a factor in monitoring the effectiveness of treatment. Although less specific, Lactate-dehydrogenase (LDH) also has prognostic value.
 |
| The cure rate for testicular cancer is quite high. |
Stages of the disease
The stages can be divided as follows: Stage T corresponds to the local spread of the tumor with 4 levels. Stage N corresponds to the spread to the retroperitoneal lymph nodes with 3 levels. Stage M corresponds to metastasis to other organs and later added stage S corresponding to specific markers (Marqueurs).
How to treat?
When diagnosing testicular cancer, orchiectomy may be indicated. After orchiectomy, prosthetic testicles should be placed in the patient to stabilize the patient's psychology. In addition, it is recommended that people who have orchiectomy should collect sperm in a sperm bank before surgery, because some drugs used to treat testicular cancer can cause sperm loss, affecting the ability to have children later. Patients should not worry too much about their sex life afterward because this surgery does not cause sexual dysfunction.
Pathological studies and assessment of the extent of localization or spread of the tumor (abdominal and thoracic CT) will help to direct the necessary additional treatment. If it is a localized testicular tumor, depending on the cell type, abdominal radiation, chemotherapy or retroperitoneal lymph node dissection, or even just routine monitoring may be recommended.
Advanced form with diffusion of cancer cells into abdominal lymph nodes or even into other organs requires multiple cycles of chemotherapy appropriate to the severity of diffusion as well as the rate of tumor marqueurs.
After chemotherapy, surgery to remove residual or metastatic lymph nodes is sometimes needed.
In the rarer situation of bilateral testicular cancer occurring simultaneously, secondary or solitary testicular cancer (only one testicle) may be a candidate for partial orchiectomy (provided the tumor is small and detected early).
The vast majority of patients are cured with the above treatments. After surgery, regular monitoring of tumor markers and CT is required.
Scrotal self-examination is recommended for all patients who have been treated for testicular cancer to detect possible recurrence early.
According to SK&DS
| RELATED NEWS |
|---|


.jpg)



.jpg)